🎉 Announcement: Official integration partner with HealthEdge GuidingCare® to automate utilization management.View announcement





Case Health AI uses proprietary AI models that work together seamlessly to handle intake, verify provider documents against criteria, and determine whether to approve, deny, or send for outreach.
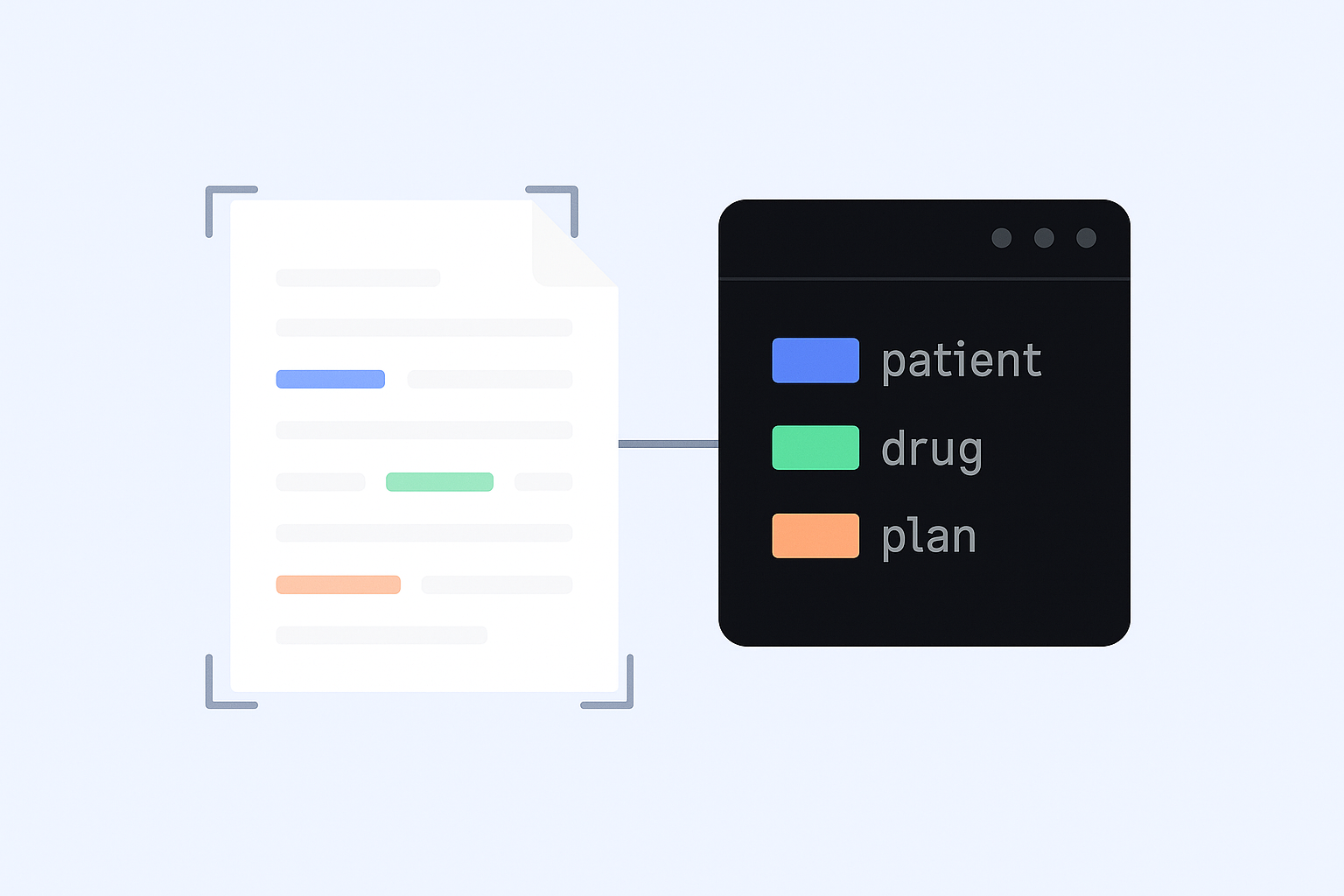
The Clinical Abstraction LLM extracts key information from any prior authorization document, including patient, provider, prescribed drug or service, and supporting diagnosis.
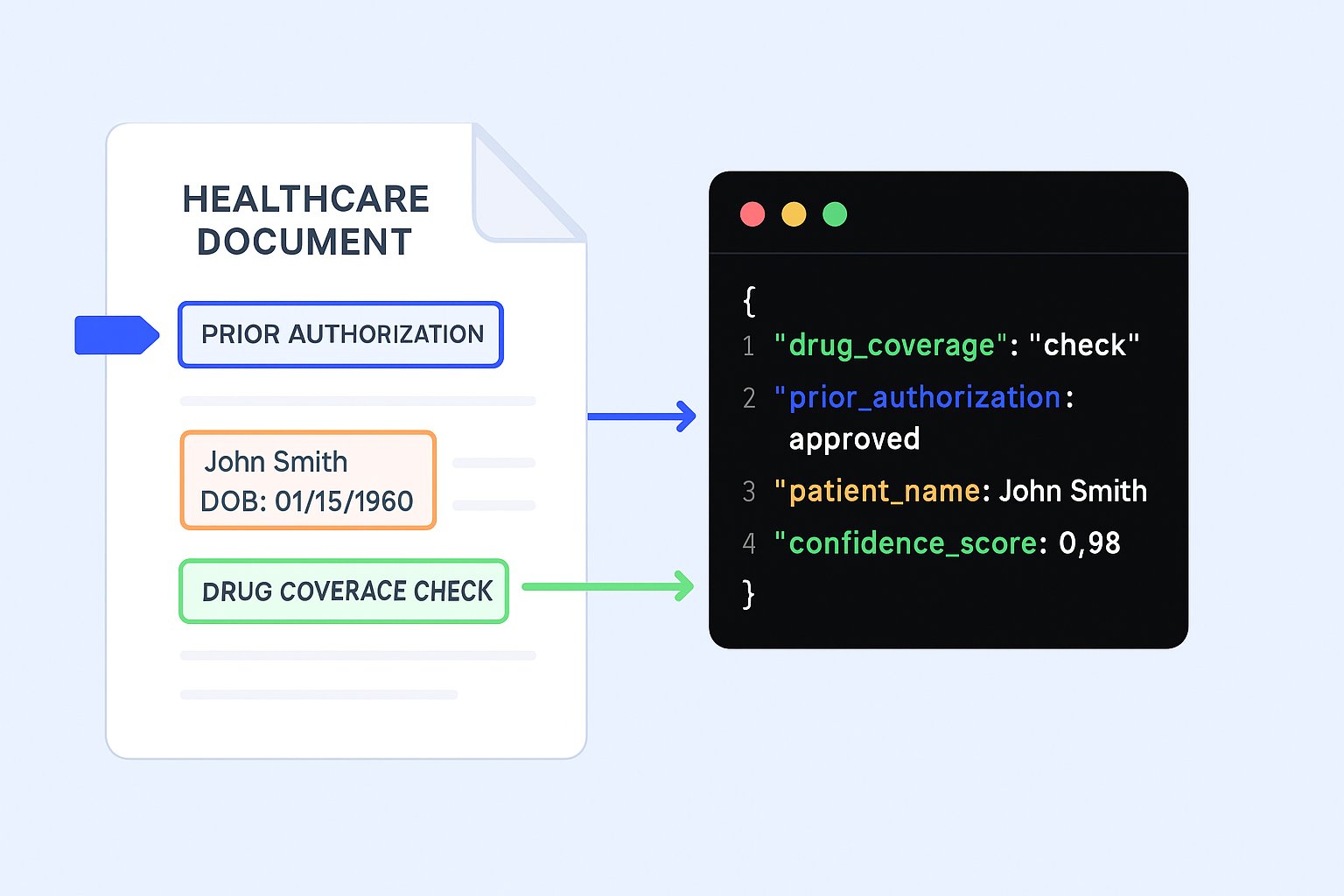
Our Evaluation LLM verifies provider documents against criteria, claims history, and payer rules to determine coverage.
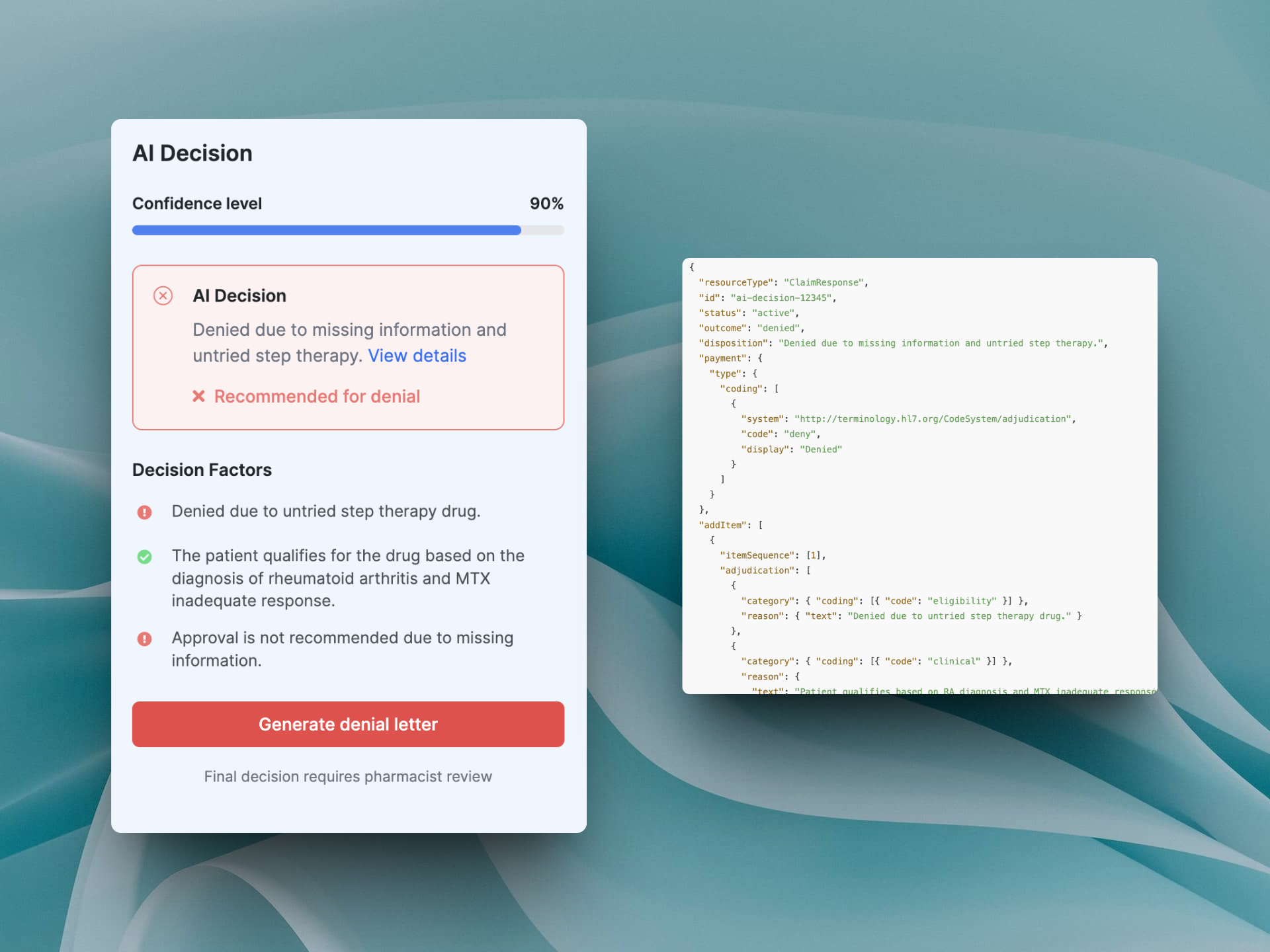
Approved cases can be sent for approval. Denied or incomplete cases return to your UM system for manual review with all intake details and criteria summaries.
Case Health AI models are trained on CMS guidelines, integrated with leading compendiums, and built by clinicians to ensure clinically accurate approvals or denials, with a complete audit trail.
Our Intake Agent, powered by CALLM™, quickly extracts every detail from a prior auth request—including codes, provider and patient info, and messy handwriting—and creates a complete case summary in under two minutes. It even detects duplicates automatically.
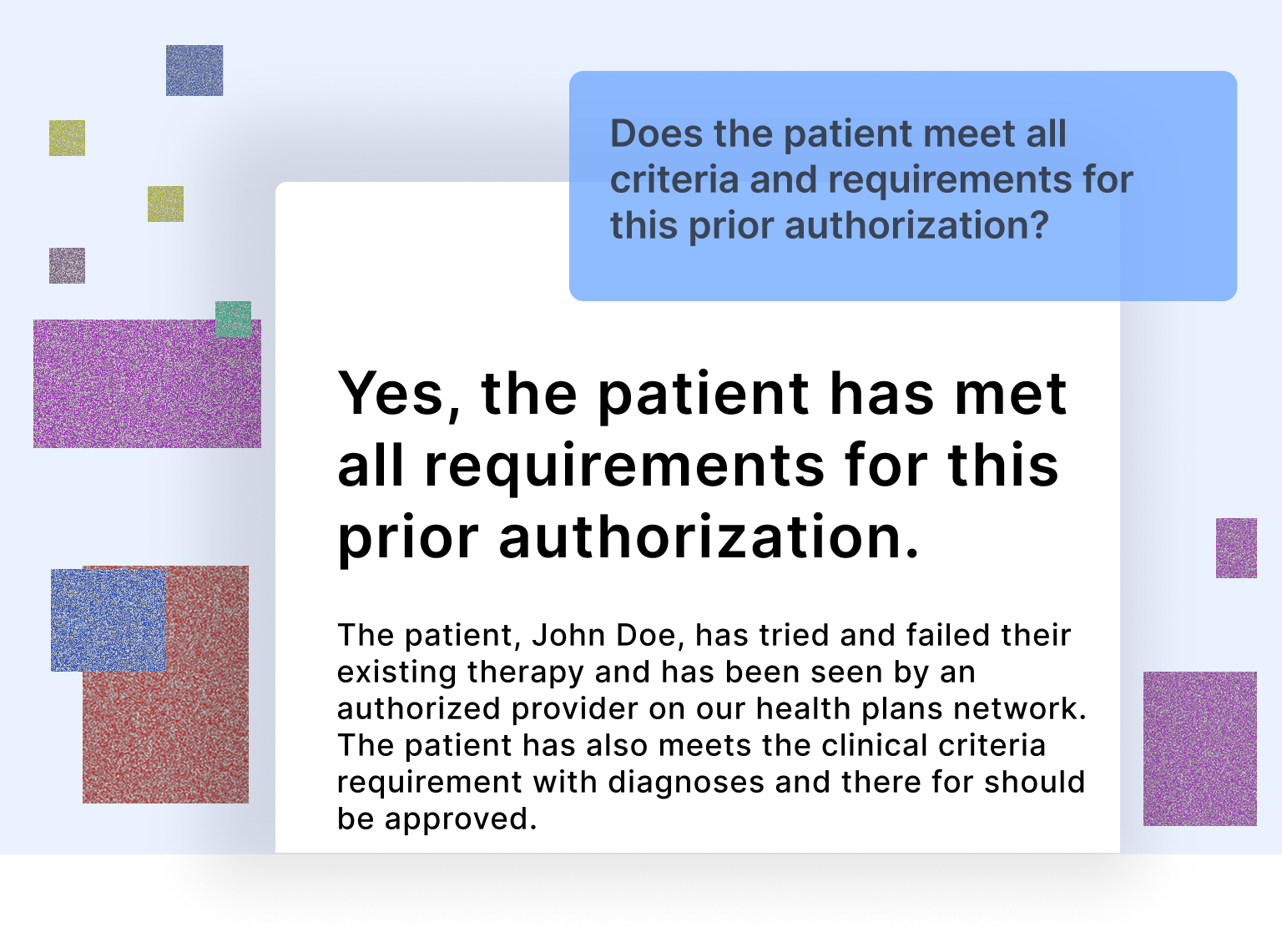
We evaluate each case using the health plan’s criteria, trusted compendiums, and the patient’s full history—including prior claims, medications, services, and past prior authorizations—powered by EVALLM to determine whether it should be approved, denied, or sent for outreach.
We send the final determination to your UM system. Approved cases can be sent for automatic approval, while denied cases go to a clinician for manual review. Intake details and criteria checks are included to help clinicians verify the AI’s decision quickly and accurately.
Our AI agents reduce friction across every step of the authorization process—cutting processing times, improving approvals, and reducing manual work. Here's what our partners have seen:
99.69%
$$$ Millions
3 min
Upload a policy in PDF or plain text — our AI parses and converts it into a structured, editable decision tree in seconds. Whether it's step therapy, tier restrictions, or prescriber rules, our system breaks it all down into clear, customizable logic blocks you can edit anytime.
Upload your prior authorization policies in PDF or text format. CHAI's AI engine will instantly convert them into structured, editable decision trees — built for speed, accuracy, and compliance. No more manual logic mapping.
Every branch in the tree is fully customizable — update conditions, reword questions, or insert new criteria anytime. Maintain control without starting from scratch.
Our AI agents use these trees to make real-time decisions. Whether it's verifying coverage rules or generating approval/denial letters, you get end-to-end automation that's explainable and auditable.
Built for enterprises—handle millions of requests with zero downtime.