Our Clinical Agent reviews diagnosis codes, patient history, and medical rationale to determine if the requested drug or service meets coverage criteria — streamlining approvals and reducing back-and-forth.
Smarter Eligibility Decisions with AI
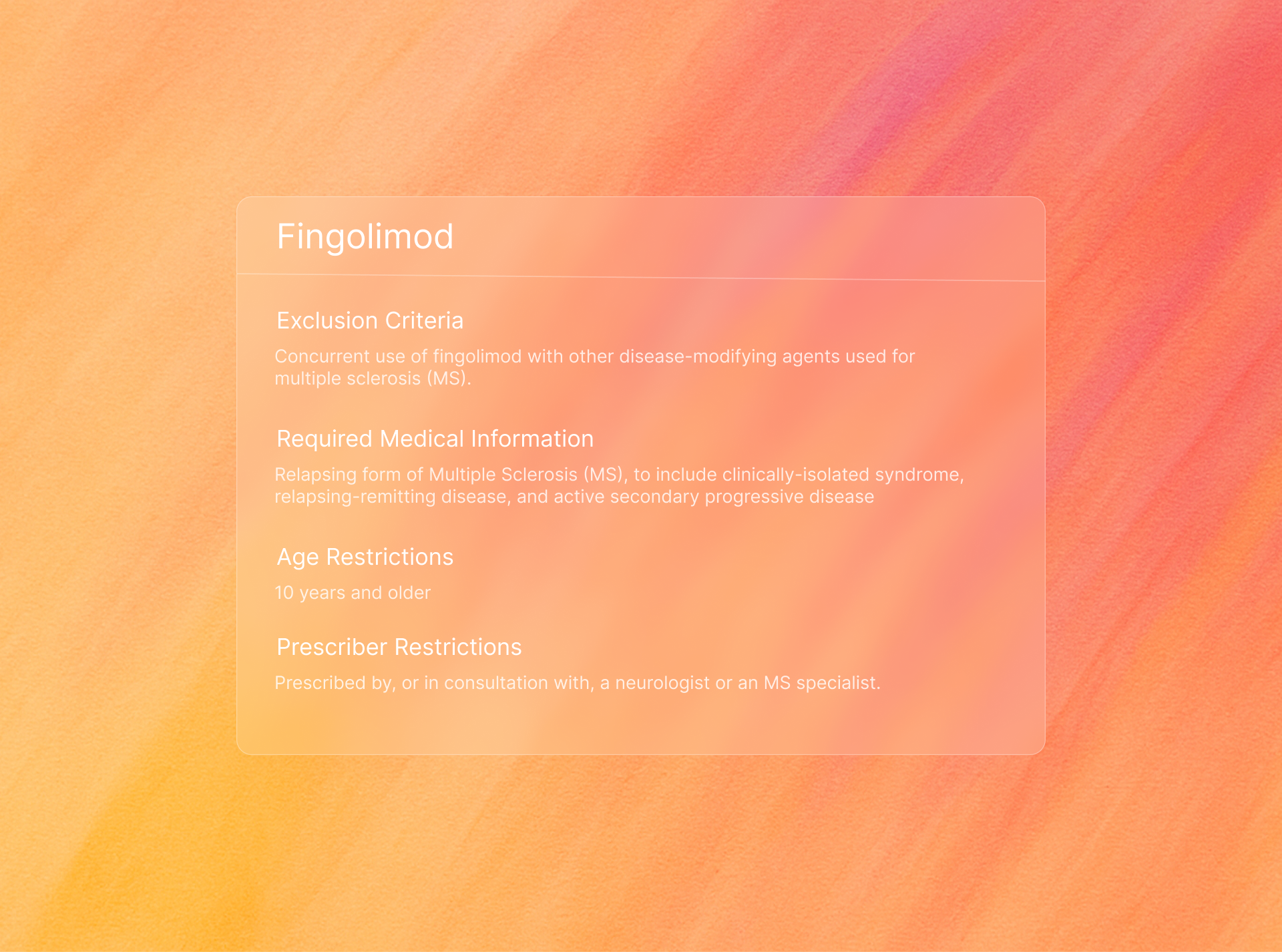
Our Eligibility Agent reads prior authorization documents to check patients eligiblity coverage, step therapy requirements, and more.
Step 1: Review Patient Case History
We parse ICD-10 codes, medical notes, and procedure history to surface relevant clinical details that support or refute the need for treatment — no chart diving required.
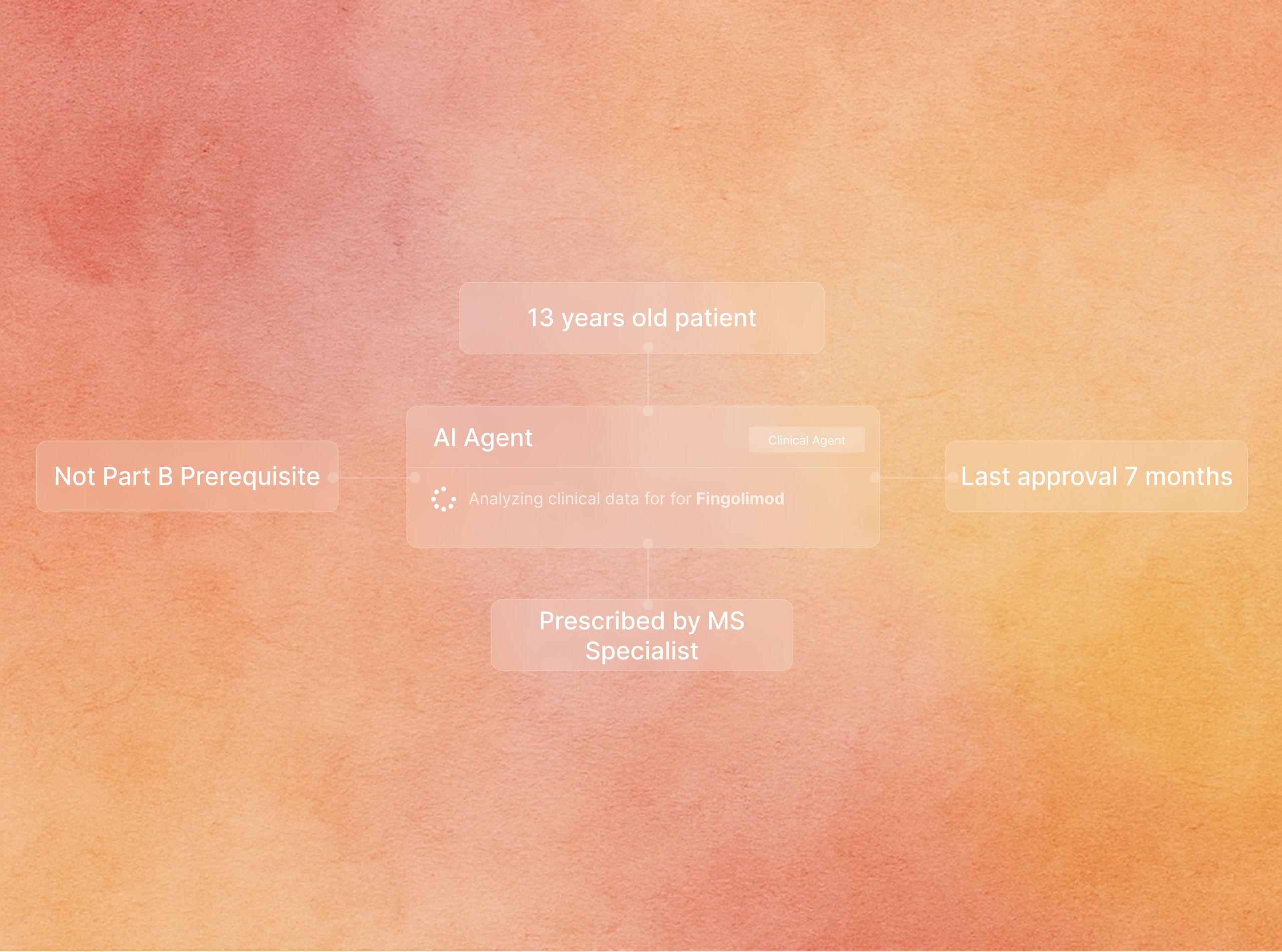
Step 2: Determine Medical Necessity
Our model maps the patient’s clinical scenario to health plan rules and evidence-based guidelines, returning a recommendation with explanation and confidence level via API.
Our AI agents reduce friction across every step of the authorization process—cutting processing times, improving approvals, and reducing manual work. Here's what our partners have seen:
95%
30%
1.5min