Instantly analyze plan formularies, benefit designs, and coverage restrictions using our Eligibility Agent — purpose-built to speed up prior authorization processing.
Smarter Eligibility Decisions with AI
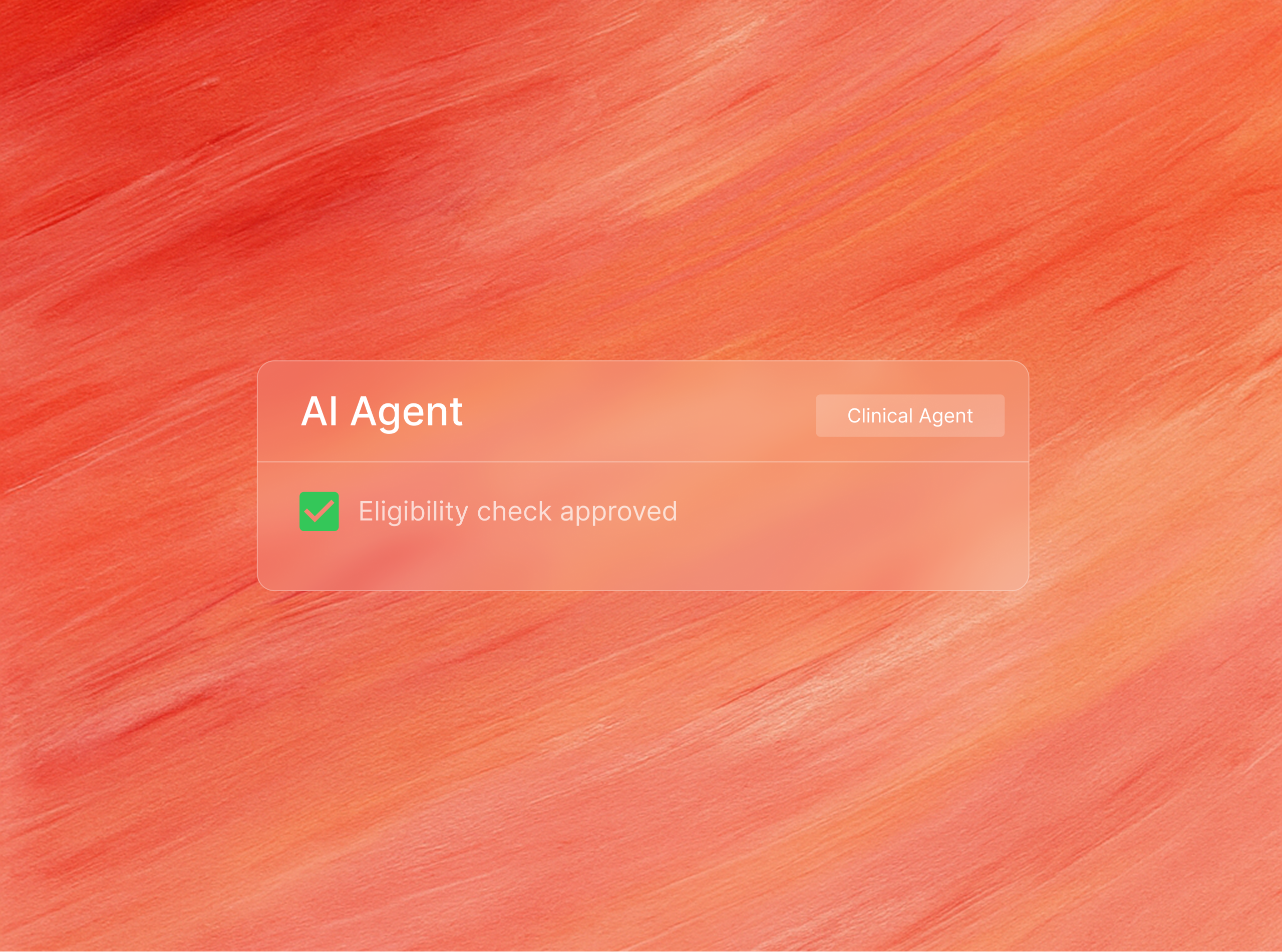
Our Eligibility Agent reads prior authorization documents to check patients eligiblity coverage, step therapy requirements, and more.
Step 1: Formulary Intelligence
Our AI reads and understands tiered coverage, step therapy, exclusions, and quantity limits directly from insurer formularies and benefit documents — turning manual reviews into milliseconds.
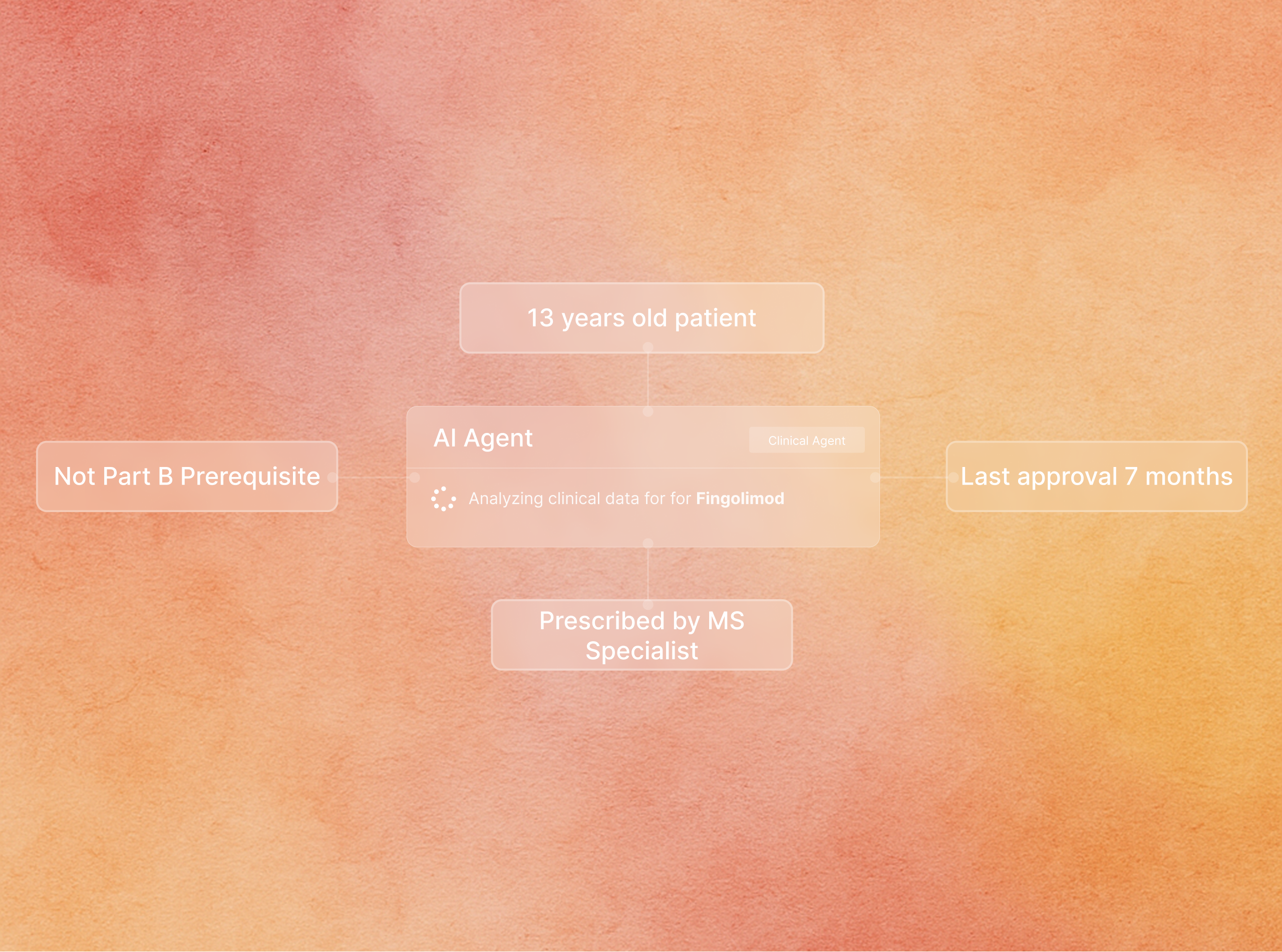
Step 2: Real-Time Coverage Checks
When given a patient’s plan and prescribed drug or service, the agent delivers a real-time verdict: covered, restricted, or not covered — with confidence scoring and explainability.
Our AI agents reduce friction across every step of the authorization process—cutting processing times, improving approvals, and reducing manual work. Here's what our partners have seen:
95%
30%
1.5min